SMR - Spinal Motion Restriction | Professional Responder Skill Series
/"Spinal Motion Restriction: Techniques and Considerations for Prehospital Care Providers"
Spinal motion restriction (SMR) is a technique used to limit movement of the spinal cord and surrounding tissues during transport to a medical facility for further evaluation and treatment. SMR is typically performed by prehospital care providers, such as paramedics or emergency medical technicians, who are trained in the technique and can quickly assess and stabilize a patient's condition.
SMR involves the use of various devices and techniques to immobilize the spine, including cervical collars, backboards, and straps. While SMR is generally considered a safe and effective method for preventing spinal cord injury, there are certain risks and considerations that must be taken into account, such as the potential for pressure ulcers, respiratory compromise, and the need for prompt removal of SMR devices once the patient reaches a medical facility. Prehospital care providers must also be aware of the latest guidelines and protocols for SMR, as these may vary depending on the patient's condition and the severity of their injuries.
In addition to trauma patients, individuals with certain medical conditions may also require SMR. For example, individuals with spinal fractures, spinal tumors, or spinal infections may require SMR to prevent further damage to the spine and surrounding tissues.
It is important to note that SMR should only be performed by trained professionals and should be used judiciously, as excessive immobilization can lead to complications such as pressure ulcers, respiratory problems, and muscle atrophy.
Ultimately, the decision to use SMR should be made on a case-by-case basis, taking into account the patient's specific needs and the risks and benefits of this technique. In some cases, SMR may be necessary for the safety of the patient, while in other cases, alternative techniques may be more appropriate.
AHS First Responder C-Spine Protocol
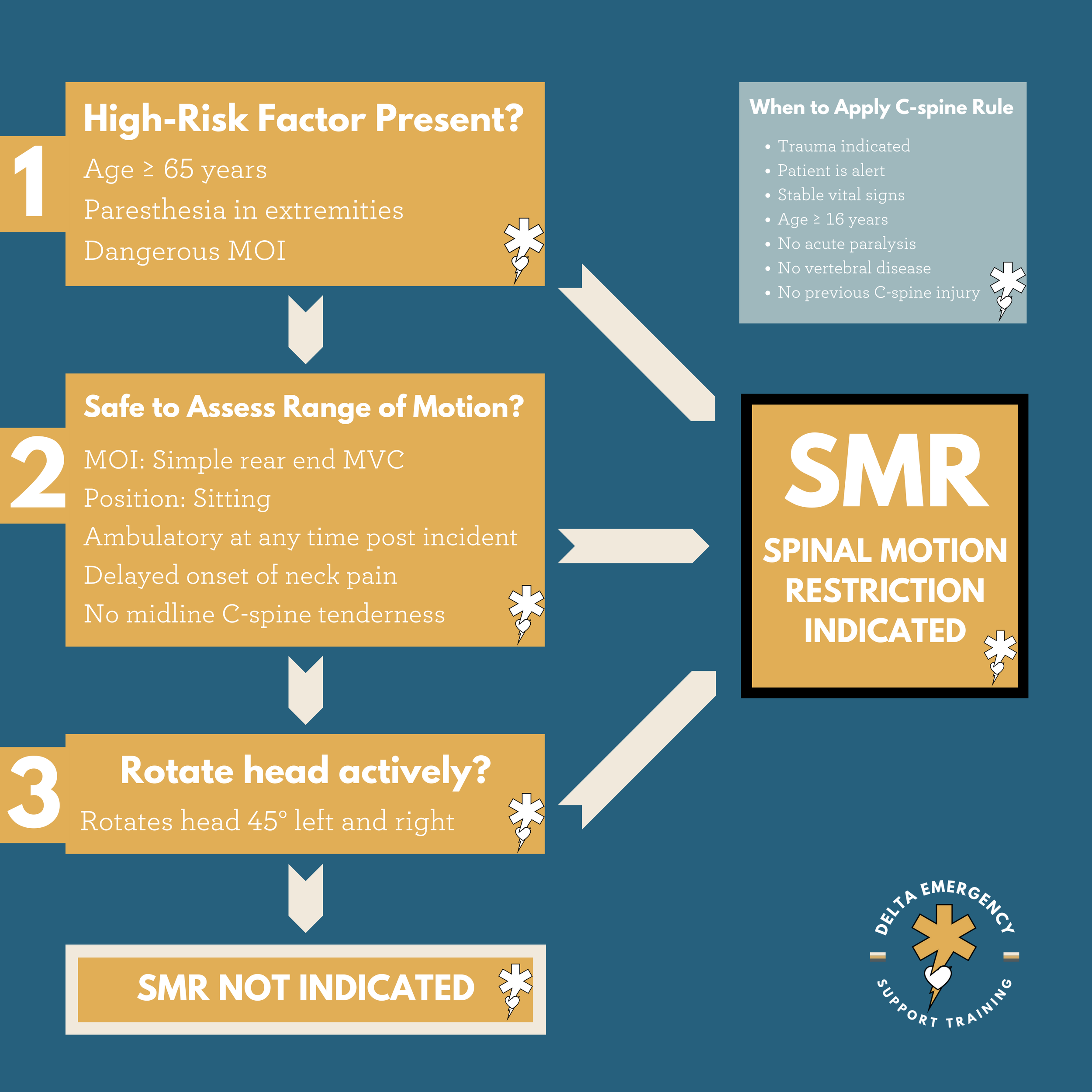
This section contains a large amount of information about how we determine applying SMR to a patient. As a firefighter or first responder in Alberta, this is the protocol you will also follow. If you examine both the Canadian C-Spine rule and the AHS C-Spine Protocol, you will find they are very similar.
Background
The C-Spine Assessment Protocol is to be applied to blunt trauma patients where there is a potential for a cervical spine injury and/or the potential for pre-hospital C-spine clearance where the practitioner needs to assess the requirement for spinal motion restriction (SMR). It is imperative that the practitioner primarily assesses the patient and not the scene or mechanism to determine the need for SMR. To facilitate this, the Canadian C-Spine Rule has been incorporated into the protocol to aid practitioners’ decision-making.
The Canadian C-Spine Rule applies to alert (GCS of 15), cooperative, and stable adult blunt trauma patients where there is a potential for C-spine injury with neck pain and/or trauma markings above the level of the clavicles.
C-collar application and SMR are contraindicated in all cases of isolated penetrating trauma. C-collar application and SMR are NEVER indicated in any isolated penetrating trauma. There is documented increased mortality due to the delay to definitive care with surgical interventions as a result of increased on scene time while applying C-collar and SMR. Of note, the long board can still be used to facilitate the extrication of the patient.
Patient Safety Considerations
SMR and C-collar application are contraindicated in cases of isolated penetrating trauma. For those patients greater than 65 years of age, take into account biological age versus chronological age. An alert, cooperative and stable patient with no neurological symptoms and no neck pain can be transported without a C-collar. The long board is not necessary for SMR
Etiology
This algorithm is designed to help the practitioner make an informed determination of the need for spinal motion restriction in the field. It is for alert (GCS of 15) and stable trauma patients where cervical spine injury is a concern.
Perform spinal motion restriction (SMR) if any of the following are present:
High-risk factors
Fall from 1 m / 5 stairs or greater
Axial load to head (e.g. diving injuries)
MVC (Speed greater than 100 km/h, rollover, ejection)
Motorized recreational vehicles
Bicycle collision with object
Medical risk factors (for example, arthritis, prolonged steroid use, degenerative bone disease, history of cervical surgery)
MVC with death of other occupant in the same vehicle
Collisions involving ATVs, motorbikes, and snowmobiles
Pedestrian/cyclist struck by motor vehicle at greater than 15 km/h
Altered LOC
Glasgow Coma Scale 14 or less
Disorientation to person, place, time, and/or event
Inability to remember 3 objects after 5 minutes
Delayed or inappropriate response to external stimuli
Paresthesia – including any abnormal motor or sensory neurological finding (e.g. numbness, tingling, weakness)
Unequal handgrip strength
Inability to raise arm(s) against gravity
Inability to move toes
Inability to perform plantar flexion and dorsiflexion of the feet
Sensory deficits such as weakness or numbness or radicular (electric or shooting) pain
Tenderness/deformity of spine
Almost all spinal injuries are associated with either pain or tenderness localized to the spine
Pain felt deeply in the neck should be considered spine pain
Alcohol/drugs affecting judgement
Communication difficulties (e.g. language barrier)
Distracting painful injury:
Long bone fracture
Abdominal or thoracic injury causing distress
Large laceration, degloving, or crush injury
Large burns
Any other injury-producing acute functional impairment
Degenerative bone disorder, ankylosing spondylitis, Down’s syndrome – assure the neutral position corresponds to the underlying medical condition
Suspicion of spinal injury on the part of the practitioner
If any of the following low-risk factors for spinal injury are present, evaluate patient for need for spinal motion restriction:
Ambulatory at any time
Absence of pain during midline palpation
Delayed (not immediate) onset of neck pain
Simple rear-end MVC, excluding:
Pushed into oncoming traffic
Hit by bus / large truck
Rollover
Hit by high-speed vehicle (100 km/hr or greater)
On evaluation, if unable to voluntarily rotate the neck 45° left and right, regardless of pain, use SMR.
Range of Motion Examination
Ask the patient to voluntarily rotate their neck 45° to the left and right regardless of pain
If the patient can rotate their neck, spinal motion restriction is not indicated\
Nerve Root | Movements
C5 | Shoulder adbuction, elbow flexion
C6 | Elbow flexion (semipronated)
C7 | Finger extension, elbow extension
C8 | Finger flexors
T1 | Small muscles of the hand
L1, L2 | Hip flexion
L3, L4 | Knee extension
L5 | Extension of great toe
S1 | Hip extension, knee flexion, plantar flexion
Don’t forget sensory — light touch/pain
Spinal motion restriction (SMR)
SMR is required in all patients with potential spinal injuries, with the exceptions as above (i.e. penetrating trauma)
Where possible, SMR should be maintained with a properly fitted C-collar and/or blanket-rolls (or a comparable commercial device) secured to the stretcher with tape when appropriate. If a c-collar would pull the patient out of neutral alignment then it should not be applied
Supine positioning is the preferred position for patients requiring SMR. However, if these patients cannot be transported supine, they should be maintained in a reasonable position of comfort with neutral alignment of the spine relative to the patient’s underlying medical condition or their current presentation
SMR should not take priority over management of life-threatening co-morbidities such as airway management or hemorrhage control
Long boards can be used for extrication or as a means of moving an immobile patient to the stretcher but is not required to achieve SMR and is contraindicated in patients who have a long transport and/or wait times (greater than 30 minutes)
EMS practitioners may remove the patient from the long board and place them supine with a C-collar and head rolls/head blocks, onto an EMS stretcher (secured with stretcher seatbelts), as soon as deemed safe and practical to do so
In cases in which SMR is indicated as per protocol, patients with life-threatening respiratory compromise exacerbated by the supine position (i.e. head, facial/neck trauma, severe respiratory disease, body habitus), may be transported on the stretcher in semi-Fowlers or high Fowlers (maintaining SMR with a C-collar/head blocks and secured with stretcher seatbelts
Patients with C-collars in place should not be transferred via wheelchair or walking
With regard to the pillow/padding of SMR patients, the priority is maintaining neutral alignment as near as possible. Continue with light padding or small pillows which do not alter the normal cervical alignment of patients as long as the SMR techniques still ensures appropriate control, immobilization and stabilization of the C-spine
Once again: C-collar application and SMR are contraindicated in all cases of isolated penetrating trauma. C-collar application and SMR are NEVER indicated in any isolated penetrating trauma. There is documented increased mortality due to the delay to definitive care with surgical interventions as a result of increased on scene time while applying C-collar and SMR. Of note, the long board can still be used to facilitate the extrication of the patient
The information above is opinion based and taken from different research articles, First Response training protocols, AHS EMS, and textbooks. There are no specifics given regarding an assessment or treatment modality, as SMR protocols change between different Fire/EMS systems. Follow YOUR local protocols.
At Delta Emergency Support Training we are happy to answer any questions you may have about spinal motion restriction. We provide training sessions for individuals or classes. We have options for in person, hybrid or online classes for Babysitters, Standard First Aid (SFA) Advanced First Aid (AFA) and Emergency Medical Responder (EMR)courses. For all inquiries please email info@deltaemergency.com